Cardiothoracic Surgery
IOACSNet
The Cardiac Surgical research programme consists of the Improving Outcomes after Cardiac Surgery Network (IOACSNet), a multi-disciplinary consortium of cardiac surgeons, anaesthetists, intensivists, clinical perfusionists and researchers involved in the care of patients undergoing cardiac surgery at public hospitals in New Zealand. IOACSNet aims to improve patient outcomes through the generation of high quality clinical evidence, particularly through the involvement of New Zealand cardiac surgical centres in high quality clinical trials and by having a structured programme for the translation of such evidence in to clinical practice.
The IOACSNet represents the fifth network within the MRINZ. The others include intensive care medicine, respiratory medicine, stroke/rehabilitation and alternative and complementary medicine.
Transfusion Medicine
The Transfusion Requirements in Cardiac Surgery III (TRICS III) Study, which was recently presented at the American Heart Association Annual meeting and simultaneously published in the New England Journal of Medicine, was conducted in 19 countries, with Dr Shay McGuinness the lead investigator in New Zealand. The study was partly funded by the Health Research Council of New Zealand and all five publicly funded cardiac surgical centres in New Zealand took part; overall these sites recruited more than 11% of the 5000 patients included. It showed that a restrictive transfusion strategy was overall no worse than a liberal strategy in patients having cardiac surgery. Secondary outcomes demonstrated that patients aged over 75 years who undergo open heart surgery are at lower risk from complications such as stroke and heart attacks if managed with a restrictive blood transfusion strategy.
The findings from the TRICS III study will be used to develop a standardised approach to blood transfusion use in patients undergoing cardiac surgery in New Zealand. It is anticipated that this will significantly decrease the amount of blood used and optimise the outcomes for patients.
Anaemia is very common in patients presenting for cardiac surgery, however both anaemia and blood transfusion are associated with worse outcomes. The Intravenous Iron for the Treatment of Anaemia before Cardiac Surgery (ITACS) Study is a NHMRC funded 1000 patient study designed to assess if the use of high dose intravenous iron reduces transfusions and complications in anaemic patients undergoing cardiac surgery. ITACS has recently commenced recruiting in Australia, New Zealand and the United Kingdom. In New Zealand ITACS is led by Dr Shay McGuinness.
Comment: ITACS will demonstrate if pre-operative intravenous iron reduces transfusions and improves patients’ outcomes and importantly includes an in depth cost-effectiveness evaluation of this therapy.
Intravenous Fluid Management
Patients undergoing surgery receive a significant amount of intravenous fluid especially immediately postoperatively in the ICU, and this is associated with worse outcomes in a variety of patient groups. We have previously documented fluid administration practice through observational studies and demonstrated in pilot work that a strategy aimed at decreasing the amount of fluid administered is effective and may lead to better clinical outcomes. The Fluid after Bypass Study (FAB study) is a multicentre Phase IIb study (n=700) designed to determine if reducing the amount of intravenous fluid given postoperatively will reduce ventilation hours and duration of ICU length of stay. Dr Rachael Parke is Chief Investigator for the FAB study which is funded by the Heart Foundation New Zealand and the Greenlane Research and Education Fund.
The FAB study is the latest phase of a programme of research investigating the use of intravenous fluids in cardiac surgical patients. Of note it is the first cardiac surgical study conceived and developed in New Zealand to involve all five publicly funded cardiac surgical centres.
Atrial Fibrillation
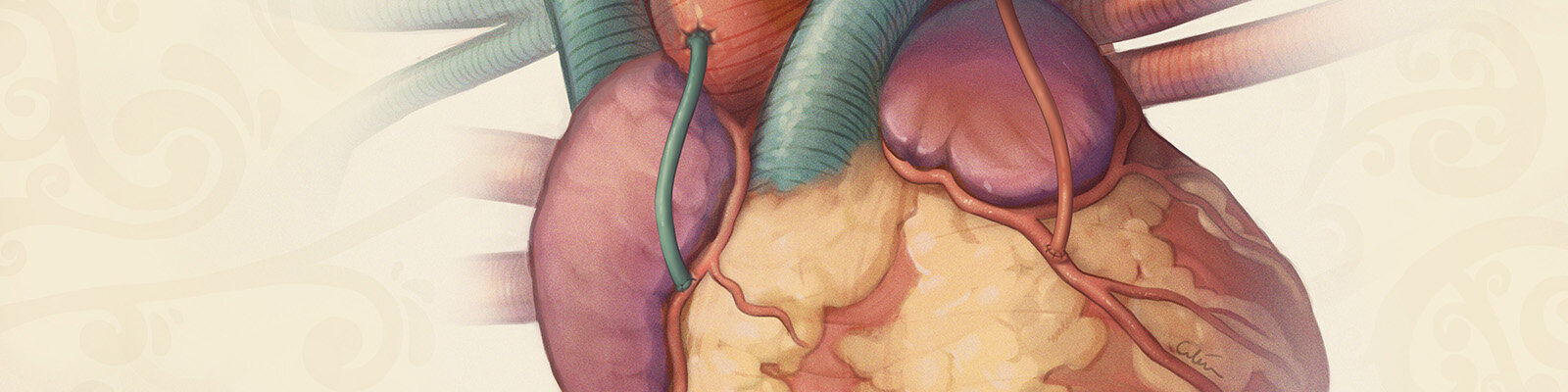
Stroke is a major and growing public health problem worldwide. In New Zealand 24 people suffer a stroke each day and almost one third will die as a result. There are significant socioeconomic and ethnic disparities – Māori and Pacifica have double the rates of stroke for people under 65 years and functional outcomes are worse. Atrial fibrillation (AF) is an important risk factor for ischaemic stroke, which accounts for >80% of all strokes. AF increases the risk of stroke five-fold and is responsible for >35% of all patients presenting with ischaemic stroke. In New Zealand the prevalence of AF is increasing and is expected to double over the next 50 years. Patients with structural heart disease have even greater risk – the combination of heart valve disease and AF results in a 17-fold increased risk of stroke and worse outcomes. New Zealand has exceptionally high rates of acute rheumatic fever, approximately 60% of whom will develop rheumatic heart disease requiring surgical repair or replacement of heart valves. The Left Atrial Appendage Occlusion III Study (LAAOS III) aims to assess if opportunistic removal of the LAA in patients with AF who are having cardiac surgery will reduce the long-term risk of stroke. It is funded by the Canadian Institute for Health Research and has 120 centres worldwide including three centres from New Zealand. It has enrolled 4000 of the target 4800 patients with recruitment expected to be completed by mid-2018.
Amputation of the LAA is a simple and inexpensive procedure if performed at the same time as open heart surgery. If it is shown to be effective in reducing stroke risk then it is likely to become a standard of care in these patients.